A Dozen States Slice Medicaid Payments To Doctors, Hospitals
By Phil
Galewitz
KHN Staff Writer
Jul 06, 2011 - Kaiser Health News
This story was produced in collaboration with USA TODAY
To contain soaring Medicaid costs, about a dozen cash-strapped states are
kicking off their new budget years by reducing payments to doctors, hospitals
and other health care providers that treat the poor.
That worries some health care experts who say the cuts, most of which went
into effect July 1 or very soon within the month, could exacerbate a shortage of
physicians and other providers participating in Medicaid.
"Further depressing payment rates can only worsen the situation," said Sara
Rosenbaum, chair of the health policy department at George Washington
University. She said some of the states cutting rates -- such as South Carolina
-- already have severe Medicaid physician shortages.
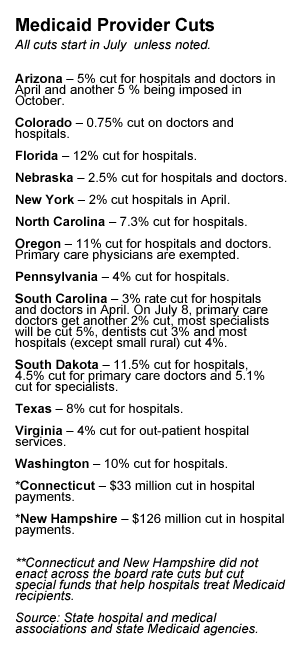
Besides South Carolina, other states that are reducing Medicaid payments to
physicians beginning in July are Colorado, Nebraska, Oregon and South
Dakota. Arizona, which cut rates in April, will impose another cut in
October. States reducing payments to hospitals include Colorado, Connecticut,
Florida, Nebraska, New Hampshire, North Carolina, Oregon, Pennsylvania, South
Carolina, Texas, Virginia and Washington. (New York cut hospital payment
rates in April).
In March, California approved a 10 percent Medicaid cut to doctors and
hospitals, but because of an existing lawsuit, those reductions are pending and
will need federal approval.
The payment cuts, which require federal approval, are part of a larger effort
by states to reduce the cost of Medicaid, typically the largest- or
second-largest expenditure after education. In some states, dental services and
other optional benefits have gone under the knife. And many states are requiring
enrollees to sign up for private Medicaid managed care plans.
Insurers and employers have their own concerns about the payment cuts. They
say trimming the rates will prompt providers to raise their prices for patients
who have private insurance. "It's always a concern that when providers get less
from Medicaid, that they will shift the costs to private insurance so families
and employers pay more," said Robert Zirkelbach, a spokesman for America's
Health Insurance Plans, an industry group.
Medicaid, a joint state-federal health care program, serves more than 50
million low-income and disabled people. Under the health care law, more
than 16 million additional people will become eligible starting in 2014, with
the federal government picking up most of the cost.
To entice more physicians to accept Medicaid patients, the law raises rates
for primary care doctors in 2013 and 2014 to match those paid by Medicare, the
federal health program for the elderly. States, on average, currently pay
Medicaid providers about 72 percent of what Medicare pays.
Medicaid enrollment shot up during the economic downturn, but $100
billion from the federal stimulus package helped states pay the tab.
However, that funding ended June 30, and now "states are struggling with what
they can do," said Laura Tobler, a policy analyst at the National Conference of
State Legislatures. The health law bars states from restricting eligibility for
the program.
Nearly half of the states cut provider payments in the fiscal year that ended
in June, according to the National Association of State Budget Officers.
But the latest cuts are among the deepest ever, say provider groups and state
officials.
© 2011 Henry J. Kaiser Family Foundation. All rights
reserved.